Damn the Mosquitoes
In recent months, officials in Brazil announced that a number of babies had been born with microcephaly.
This week, the director of the U.S. Centers for Disease Control and Prevention (CDC) declared there is sufficient evidence to link microcephaly with Zika, a virus born by the Aedes aegypti mosquito. This news is causing a stir in the Americas, but the numbers of those affected are still modest. As of March 2016, 907 children show characteristic signs of microcephaly in Brazil.
Compare this with an anopheles mosquito-born parasite, malaria. Right now, 3.2 billion human beings are currently at risk of infection. In 2015, 214 million were infected, and 438,000 of them did not survive. Malaria infection in pregnancy is responsible for one in five stillbirths in sub-Saharan Africa, and 100,000 newborn deaths each year. The difference in global impact couldn’t be more pronounced. What might seem a disproportionate amount of fear for the newer mosquito-born illness might be explained simply: “better the devil you know than the devil you don’t.”
Zika isn’t new. It first showed up in 1947, and has continued to pop up around the globe since. Malaria, on the other hand, has a much longer, deadlier history. The CDC estimates the parasite has been spread for around four thousand years. King Tut is said to have died of malaria as a young man. References to it can be found in historical writing from China to Rome. Today nine out of 10 people who die of malaria live in sub-Saharan Africa. The majority of those who die are children under five years of age. So why isn’t it a problem in the United States? If we eliminated malaria here, can’t we do it with Zika? Don’t we have medicine and chemicals to control and kill insects? A look at the history of fighting mosquitoes tells us that chemical and biomedical interventions won’t do the job alone: human behavior needs to change.
Since 1880, a tremendous amount of work has gone into killing mosquitoes, adapting our environment and sleeping spaces to keep them away, all while consuming lots and lots of drugs to prevent and treat infection. Times have changed, however, and while humans are still busy spraying chemicals, the ones that still work are having difficulty keeping up with mosquito resistance. Sleeping under insecticide-treated nets still works, but as resistance to chemicals builds, the intervention may serve as a barrier, rather than a mosquito killer. Scientists have produced one treatment drug after another as resistance to each develops. Even as each method of fighting mosquitoes is being adapted, and scientists race to keep up, the international community has committed to eliminating malaria. If our chemical and biomedical solutions are busy running on a treadmill ahead of resistance, what makes anyone think malaria elimination is possible?
This year has been a year of new malaria strategies. The WHO released one strategy, the Roll Back Malaria Partnership rolled out their supporting strategy, and the President’s Malaria Initiative released their own. All three of these strategies align with the newly released global development strategy, the Sustainable Development Goals. These documents point out that amazing progress has been made. They also acknowledge that the political will and financial commitment that got us this far can’t stop now, or these fragile gains will not be sustained.
So I’ve adapted that old saying – Damn the Torpedoes (Mosquitoes) – full speed ahead!
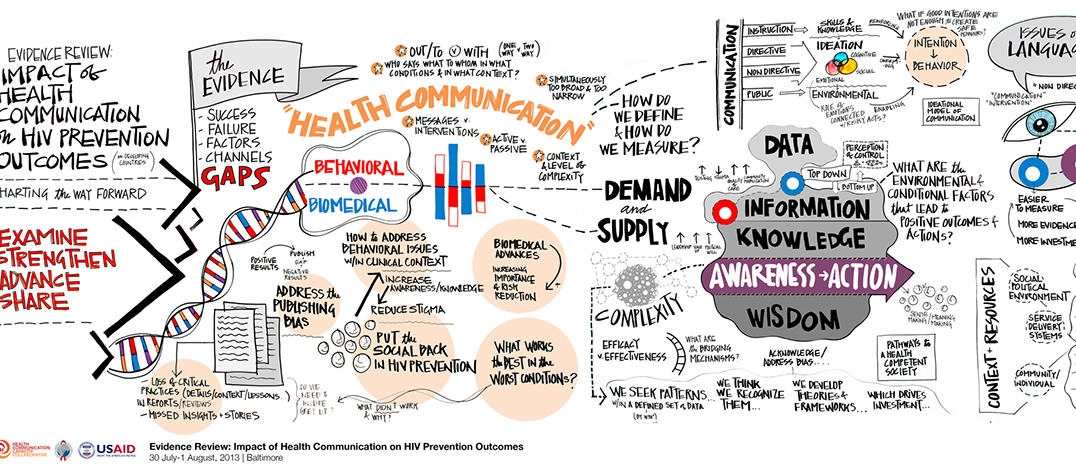
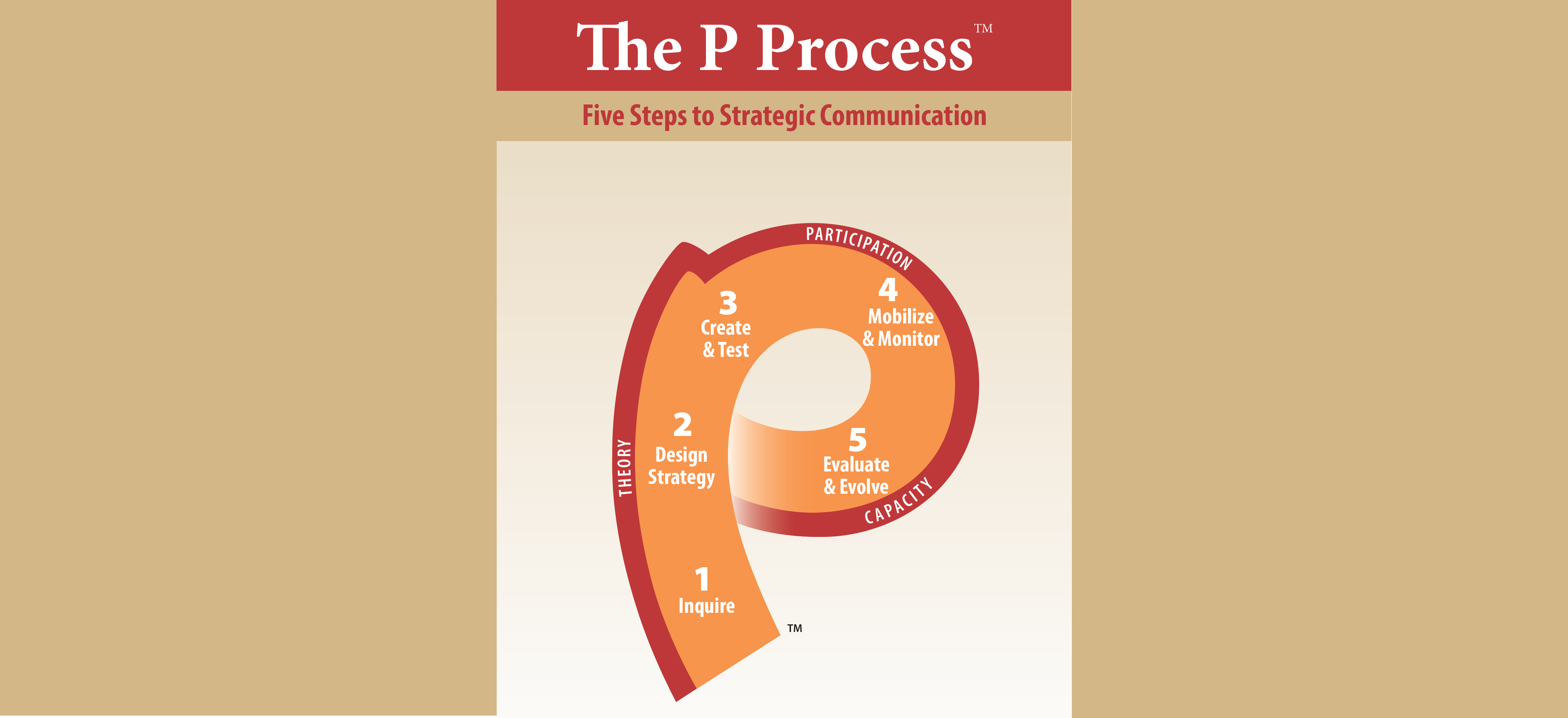
One way to build on gains made in the fight against malaria will be to increase the level of engagement between donors, program managers and the people living in communities affected by malaria. The new RBM strategy calls this “keeping people at the center of the response.”
“To achieve the 2030 malaria goals, we need to put the people that live in affected communities at the center of all efforts to scale up the design and delivery of malaria services. Far from being the optional “extra,” people need to be our first point of reference when it comes to analyzing the barriers to access, product or strategy design; piloting; implementation; feedback, learning and monitoring.”
This focus is refreshing. Boatloads of chemicals, shipments of rapid diagnostic tests and drugs and all of the long-lasting insecticide-treated nets in the world will do little if the communities living with malaria do not trust in their safety and efficacy and use them. Continued political will and financial resources to provide these life-saving commodities is essential, as are renewed efforts to encourage demand and use among those they are intended to benefit. April 25 is World Malaria Day. Leaders from around the world are coming together to declare we will “Defeat Malaria, For Good.” With renewed focus and commitment, and more robust focus on community engagement, we can be the generation to end one of the oldest and deadliest diseases in human history.
What is your country doing to “end malaria for good”? Does your organization have experience conducting SBCC for elimination? Join moderators Andrew Tompsett (PMI), Mike Toso (HC3), Rebecca Shore (VectorWorks) and Bill Brieger (Johns Hopkins University) for a conversation on April 25-26 around has social and behavior change communication been integrated as part of the solutions and strategies needed in the malaria fight to the final mile to elimination? If not, what needs to done?






Leave a Reply
Want to join the discussion?Feel free to contribute!