Health Communication Leads to Better Outcomes for Those Receiving HIV Treatment
Effective health communication helps keep people in treatment throughout the HIV continuum of care, thus leading to more positive health outcomes, according to a new supplement of the Journal of Acquired Immune Deficiency Syndromes (JAIDS).
 The just-published JAIDS supplement follows the July 2014 edition (Health Communication Strategies in Combination HIV Prevention and Care Programs) that provided evidence of health communication’s positive impact on HIV prevention, care and treatment. Both supplements were sponsored by the Health Communication Capacity Collaborative (HC3), a five-year global communication project funded by the U.S. Agency for International Development (USAID) through the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) and based at Johns Hopkins Center for Communication Programs (CCP).
The just-published JAIDS supplement follows the July 2014 edition (Health Communication Strategies in Combination HIV Prevention and Care Programs) that provided evidence of health communication’s positive impact on HIV prevention, care and treatment. Both supplements were sponsored by the Health Communication Capacity Collaborative (HC3), a five-year global communication project funded by the U.S. Agency for International Development (USAID) through the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) and based at Johns Hopkins Center for Communication Programs (CCP).
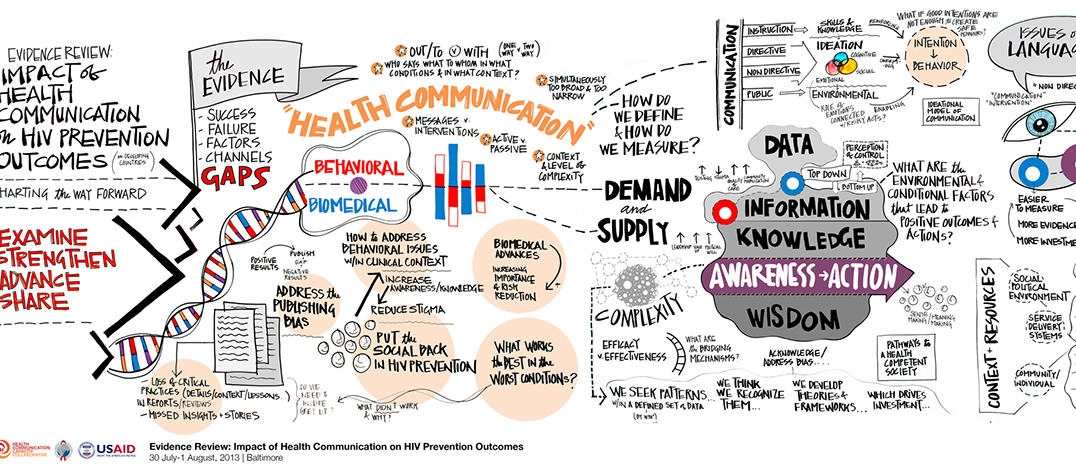
The HIV continuum of care begins with HIV testing, linking those who test positive to care, treatment initiation and ongoing adherence and retention in care with the aim of achieving viral suppression. Health communication plays an important role at every step to keep people living with HIV engaged in care and healthy.
“Health communication can motivate people to get tested, get treated and stay on treatment for the rest of their lives. That’s because health communication seeks to address frankly the complex behaviors that influence HIV-related decision-making in the context of HIV,” said the supplement’s co-guest editor, Sten Vermund, MD, PhD, professor and director of Vanderbilt University’s Institute for Global Health. Helen Struthers, PhD, chief operating officer at Anova Health Institute in Johannesburg, South Africa, served as the other co-guest editor.
Health communication can help minimize significant losses at each stage of the HIV continuum of care, thereby contributing to achieving the 90-90-90 global treatment goal set by the Joint United Nations Program on HIV/AIDS and supported by PEPFAR. As the World Health Organization recommendation of treatment for all as soon as possible after testing positive rolls out, the role of health communication will continue to play a crucial role in reaching those most in need and supporting them along their treatment journey.
This JAIDS supplement presents a series of 10 articles that make the case for using health communication in highly diverse HIV contexts in low and middle income settings. The opening article – by lead author Stella Babalola, PhD, Associate Professor at Johns Hopkins Bloomberg School of Public Health – provides a foundation for understanding why health communication leads to successful outcomes along the HIV continuum of care.
Subsequent articles provide real-world examples from Kenya, Lesotho, Mozambique, Senegal, South Africa, Tanzania and Uganda where health communication made a measurable difference in HIV treatment outcomes.
For example, The Potential Impact of Integrated Stigma Mitigation Interventions in Improving HIV/AIDS Service Delivery and Uptake for Key Populations in Senegal – by Carrie Lyons, MPH, and Stefan Baral, MD, MPH, MBA, both with the Bloomberg School – demonstrates how a program aimed at mitigating HIV stigma in Senegal led to less fear in seeking health services over time among men who have sex with men and female sex workers. Other authors include Sosthenes Ketende, MSc, Benjamin Liestman, MSPH, and Karleen Coly, MA, all with the Bloomberg School.
Another article entitled Effective Interpersonal Health Communication for Linkage to Care following HIV Diagnosis in South Africa evaluated a program in South Africa that promoted “precision health communication” between health care providers and clients to address individual client concerns about accessing care. The article was written by Tonderai Mabuto and Salome Charalambous, both with The Aurum Institute and University of the Witwatersrand School of Public Health in Johannesburg, South Africa, along with co-author Chris Hoffmann, MD, MPH, with the Johns Hopkins University School of Medicine and the Bloomberg School.
Several other articles in the supplement may be accessed directly here: http://journals.lww.com/jaids/toc/2017/01011.
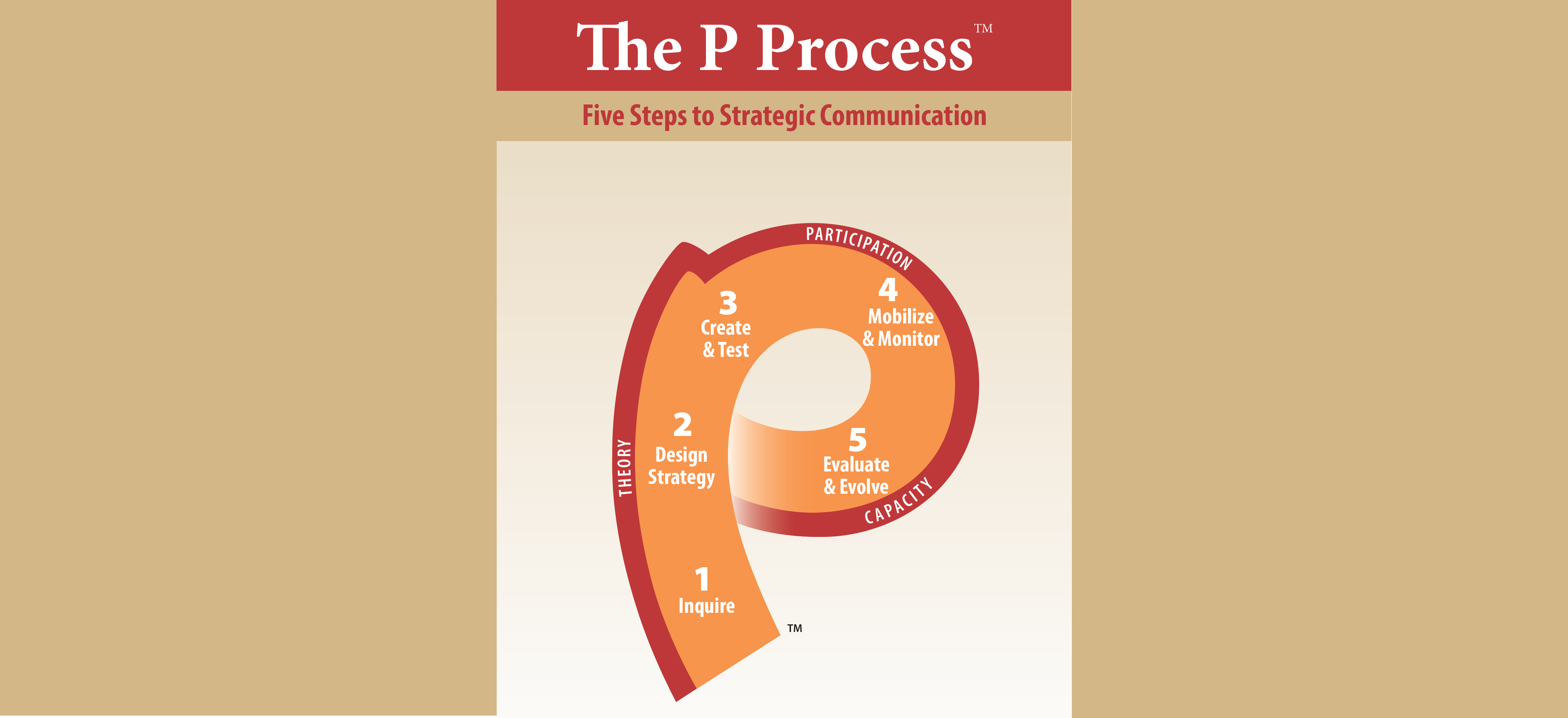
USAID-funded HC3 is designed to strengthen capacity to implement state-of-the-art health communication programs. Among the important health areas addressed by HC3 are family planning and reproductive health; maternal, neonatal and child health; HIV; malaria; and infectious diseases such as Zika and Ebola. It is led by CCP in collaboration with Management Sciences for Health, NetHope, Population Services International, Ogilvy Public Relations and Internews. HC3 is also linked to a network of organizations throughout Africa, Asia and Latin America.
An event was held on December 13 with selected authors from the supplement. More information and a link to the recorded event can be found here.
Articles Included in the Supplement:
|
|
A framework for health communication across HIV continuum of care and treatment
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|





Leave a Reply
Want to join the discussion?Feel free to contribute!