New Study Shines Light on Healthy Timing and Spacing of Pregnancy for Postpartum Women

A 20-year-old implant user from Bangladesh sits with her local Field Worker Assistant at a group talk discussing family planning options.© 2011 Lynn M. Van Lith, Courtesy of Photoshare
Postpartum women are among those with the highest unmet need for family planning, yet few studies have demonstrated how family planning services can be integrated with maternal and neonatal care to meet their needs. The Healthy Fertility Study (HFS) set out to do just that. A recent article by Ahmed and colleagues, published in the Global Health: Science and Practice journal, maps out an intervention design for an integrated, community-based program in Bangladesh for postpartum family planning and maternal and newborn health.
Data from the project’s formative research was striking – risk perception and awareness of benefits was high, and there was an expressed desire for birth spacing among postpartum women, yet social norms around closely spaced pregnancies appears to be driving behavior.
The consequences of closely spaced pregnancies are profound for maternal, perinatal and neonatal outcomes: birth-to-pregnancy internals shorter than 24 months are associated with increased risk of stillbirth, prematurity, low-birth weight and neonatal mortality, as well as maternal mortality, pre-eclampsia, induced abortion and miscarriage. The greatest risks present when the birth-to-pregnancy interval is less than six months. In response, a WHO Technical Consultation on Birth Spacing in 2005 recommended spacing pregnancies at least 24 months after the preceding birth and waiting at least six months after miscarriage or induced abortion. Timing pregnancies after age 18 and before age 34, and limiting the total number of children are also important to reduce adverse outcomes.
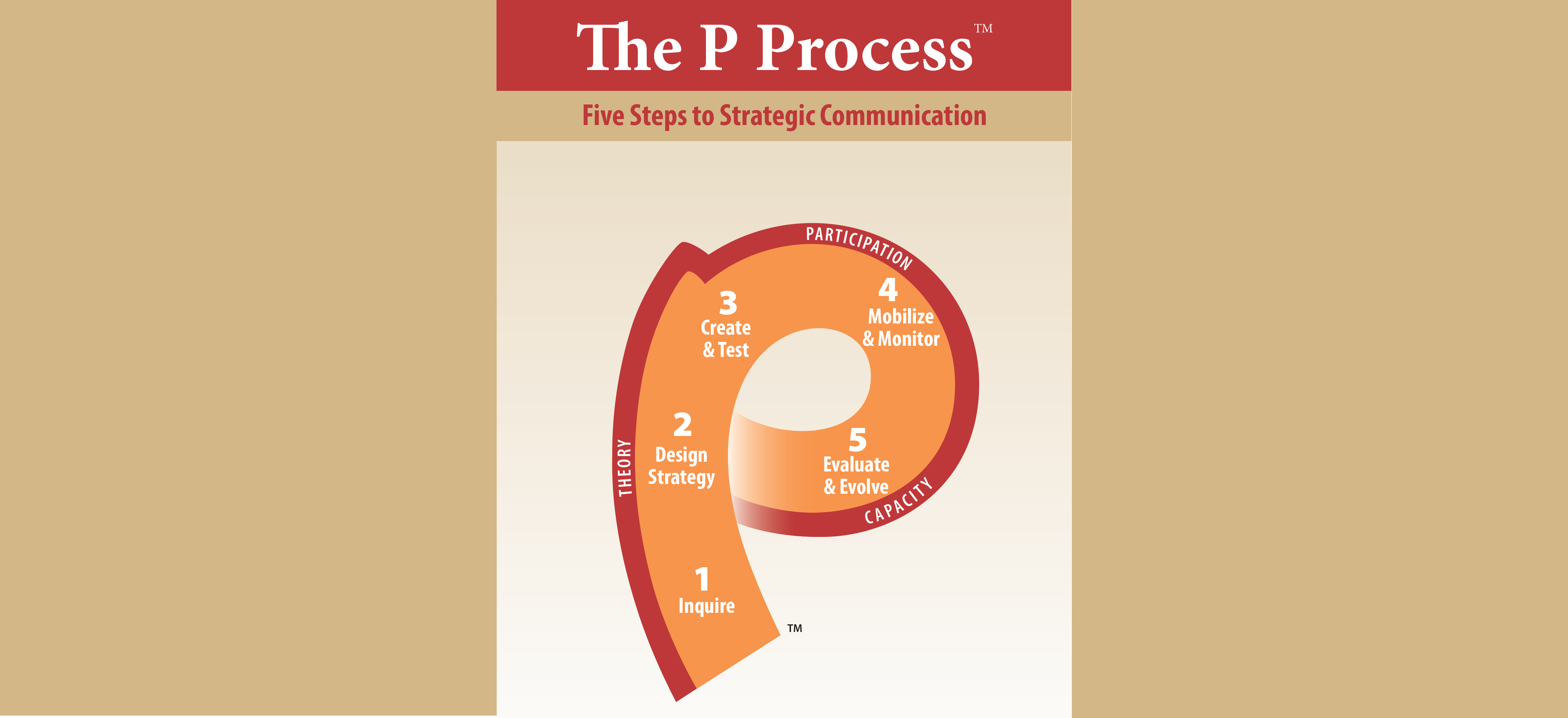
The HFS focused on three key elements: (1) more clearly specifying the healthy behaviors needed to achieve birth-to-birth intervals of at least three years; (2) reinforcing risks and benefits; and (3) providing integrated services through community health workers (CHWs). Promotion of Lactational Amenorrhea Method (LAM) during the first six months and transition to another modern method was central to each element.
Although results from the project evaluation are not yet available, this article provides a closer look at an integrated, community-based program, including the design and development of communication programming. Using a combination of CHW outreach and community mobilization, the HFS is reaching women, their families and their communities with life-saving knowledge and community-based provision of MNCH and FP services. Rather than trying to reach all women, this project sets itself apart from many other integrated programs by targeting pregnant and postpartum women.
In the coming year, HC3 will itself be focusing on building capacity in strategic behavior change communication for HTSP. We will be looking out for the new knowledge and insight that the HFS evaluation data will bring.





Leave a Reply
Want to join the discussion?Feel free to contribute!